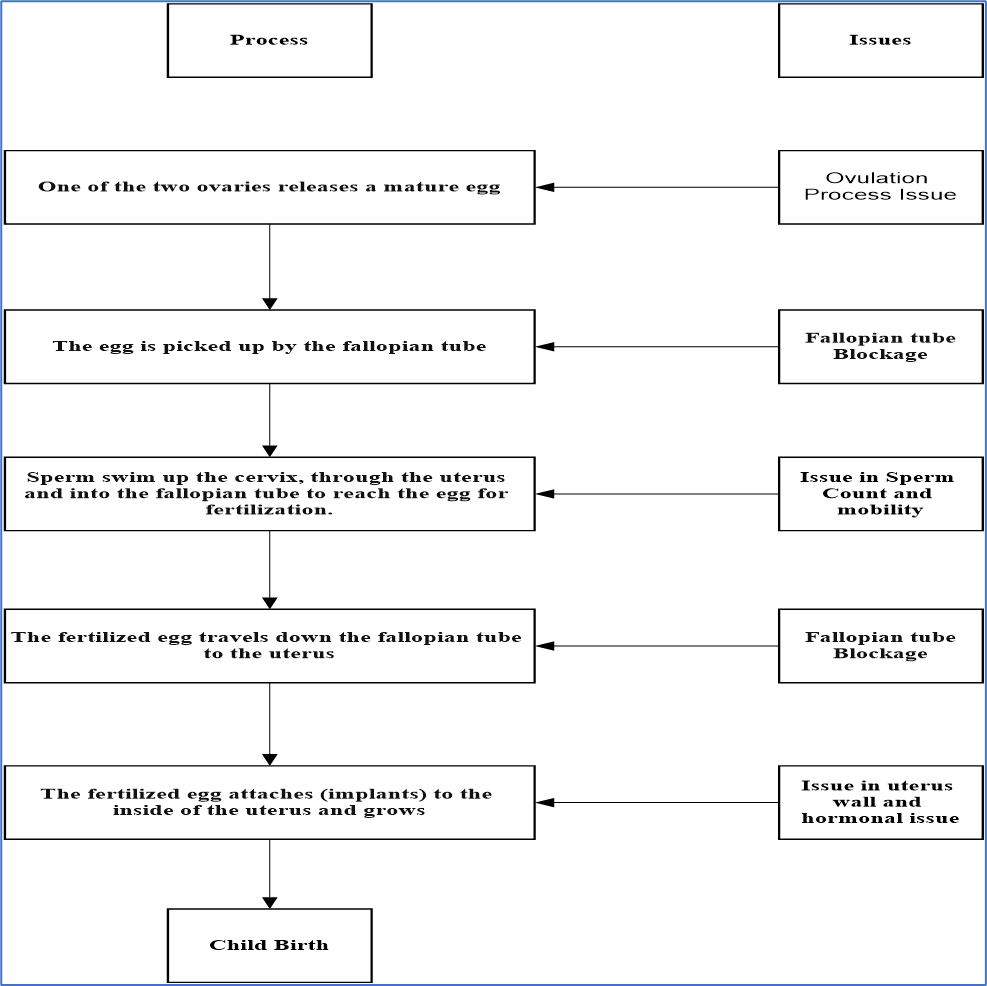
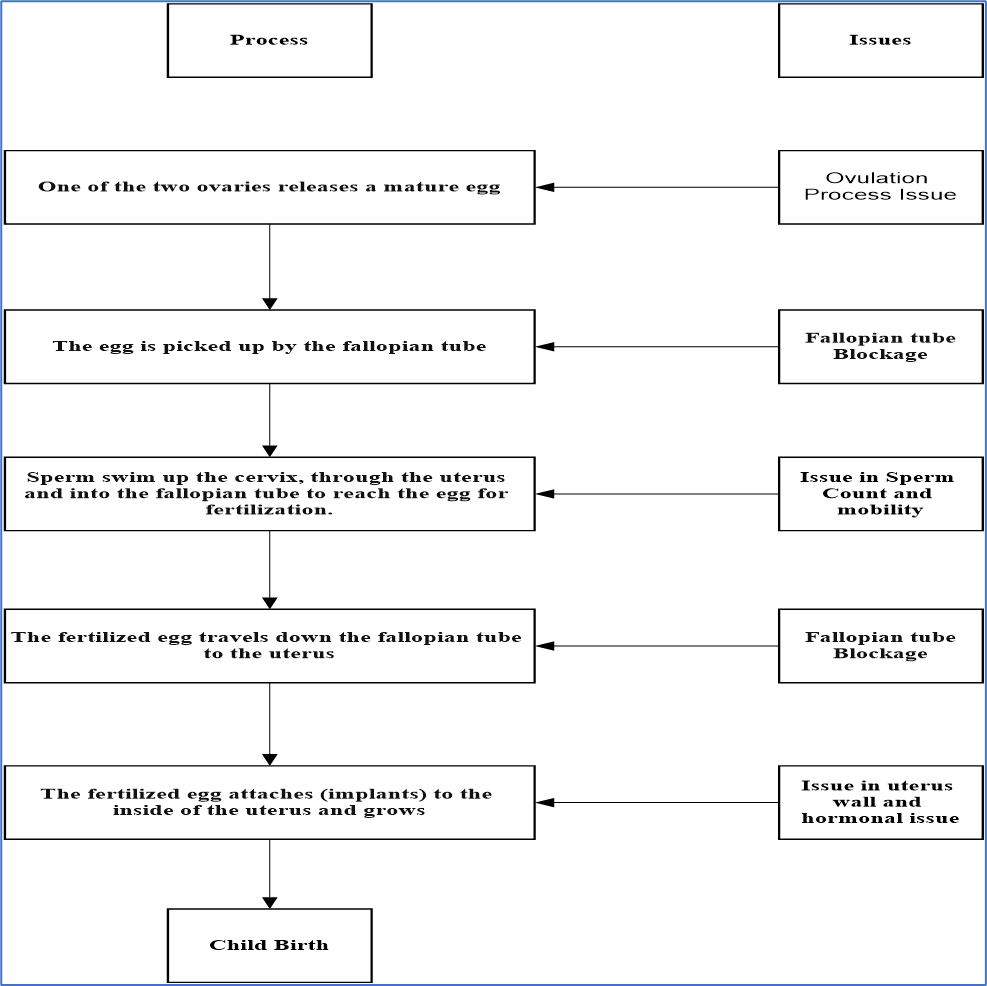
What is the ideal process to conceive the child?
What are the causes for Female infertility?
A. Ovulation disorders
- The common of cases of infertility are caused by ovulating irregularly or not at all. Ovulation abnormalities can be caused by issues with the hypothalamus or pituitary gland’s management of reproductive hormones, as well as issues with the ovary.
- Polycystic ovary syndrome (PCOS):
- PCOS reasons for a hormone imbalance, which affects ovulation. Read more on PCOS.
- Hypothalamic dysfunction
- Each month, the pituitary gland produces two hormones that help to stimulate ovulation: 1. Luteinizing hormone (LH) and 2. Follicle-stimulating hormone (FSH).
- Extra physical or emotional stress, an extremely high or extremely low body weight, or a recent significant weight gain or loss can all alter hormone production and impact ovulation. The most prevalent symptoms are irregular or interrupted menstruation.
- Primary ovarian insufficiency
- Premature ovarian failure, also known as autoimmune ovarian failure, is caused by an autoimmune response or the premature loss of eggs from your ovary, which can be caused by genetics or chemotherapy.
- In women below the age of 40, the ovary no more produces eggs and estrogen production is reduced.
- High prolactin
- The pituitary gland can produce an excess of prolactin (Known As: Hyperprolactinemia), which decreases Estrogen production and can leads to infertility. This may also be done by medications taken for another condition.
B. Blockage or damage to female fallopian tubes (tubal infertility):
- Damage or obstruction of the fallopian tube can be caused by a variety of factors:
- Pelvic inflammatory disease,
- Chlamydia, gonorrhoea, or other sexually transmitted illnesses infect the uterus and fallopian tubes.
- Previous abdominal or pelvic surgery, such as surgery for ectopic pregnancy, which occurs when a fertilised egg implants and grows elsewhere other than the uterus, generally in a fallopian tube.
C. Endometriosis:
- Endometriosis is a condition in which tissue that normally grows in the uterus implants in other parts of the body. Scarring from this extra tissue growth, as well as its surgical removal, can obstruct fallopian tubes, preventing an egg and sperm from combining.
- Endometriosis can possibly stop the fertilized egg from implanting. The illness’s indirect impacts, such as sperm or egg damage, appear to have an influence on fertility.
D. Uterine or cervical causes
Several uterine or cervical factors can prevent the egg from implanting or raise the chances of miscarriage:
- In the uterus, benign polyps or tumors (fibroids or myomas) are frequent. Some of them can block fallopian tubes or hinder implantation, lowering fertility However, many women with fibroids or polyps do get pregnant.
- Problems with the uterus, like an abnormally shaped uterus, could make it difficult to be pregnant or stay pregnant.
- Cervical stenosis is a narrowing of the cervix caused by a genetic abnormality or cervix damage. Cervical mucus problems also effect.
- The cervix doesn’t always create the right type of mucus to allow sperm to pass through and enter the uterus.
- Pelvic inflammatory disease (PID)
E. Unexplained infertility :
- The cause of infertility is sometimes never discovered. Unexpected reproductive issues could be caused by a combination of small variables in both couples. Although it’s aggravating to receive no precise response, this issue will eventually resolve itself. Infertility therapy, on the other hand, should not be put off.
F. Medicines and drugs
Adverse effects of some types of medicines and drugs may cause infertility:
- Non-steroidal anti-inflammatory drugs (NSAIDs) : Long-term use or a high can make it more difficult to conceive
- Chemotherapy: It will affect ovaries to perform better.
- Neuroleptic medicines: These drugs may cause of missed periods or infertility
- Spironolactone
- Illegal drugs: It can extremely affect fertility and make ovulation more problematic.
G. Sterilisation
- If a woman does not wish to have any more children, she may choose to be sterilised.
- The fallopian tubes are blocked during sterilisation, making it impossible for an egg to reach the womb.
- It’s seldom reversible, and even if it is, you won’t always be able to have a child.
What are the Risk factors for female infertility?
Risk factors include as below but it should be diagnosed with proper medical observation:
- Age
- The quality and quantity of a woman’s eggs start to decline as she gets older. The rate of follicle loss accelerates in the mid-30s, leading to fewer and lower-quality eggs.
- This makes it more problematic to conceive and raises the chances of miscarriage.
- Smoking
- Smoking raises your chances of miscarriage and ectopic pregnancy, in addition to harming your cervix and fallopian tubes.
- It’s also known to prematurely age the ovaries and reduce the quality of your eggs. Before starting fertility treatment, you need to quit smoking.
- Weight
- Ovulation might be hampered by being overweight or considerably underweight.
- Increase the frequency of ovulation and the likelihood of conception by achieving a healthy body mass index (BMI).
- Sexual history
- The fallopian tubes can be damaged by sexually transmitted illnesses including chlamydia and gonorrhoea.
- Having unprotected intercourse with several partners raises your risk of contracting a sexually transmitted infection, which can lead to fertility issues in the future.
- Sexually transmitted infection (STI).
- Alcohol
What is the prevention step for female infertility?
These suggestions may be useful for ladies who are planning to become pregnant soon or in the future:
- Keep a healthy weight:
- Ovulation problems are more frequent in overweight and underweight women. Moderate activity is suggested if you need to lose weight.
- Stop smoking:
- Tobacco has a number of harmful impacts on fertility, general health, and the health of a fetus. Time to quit smoking if you are planning for the family.
- Avoid alcohol
- To much drinking can lead to a loss of fertility. Any alcohol consumption during pregnancy might have a negative impact on the fetus’s health.
- Avoid alcohol if you’re planning to become pregnant, and don’t drink while you’re pregnant.
- Maintain stress:
- Research has shown that stress can affect couples’ to have poorer results with infertility treatment.
- Reduce stress in routine life before trying to become pregnant.
How to diagnosed female infertility?
Fertility tests might include:
- Ovulation testing
- The rise in luteinizing hormone (LH) that occurs before ovulation is detected by an at-home, over-the-counter ovulation prediction test. One can also confirm if patients ovulating with a blood test for progesterone, a hormone produced after ovulation. Other hormone levels, such as prolactin, may be tested as well.
- Hysterosalpingography
- X-ray contrast is injected into your uterus during hysterosalpingography, and an X-ray is obtained to check for issues inside the uterus.
- Ovarian reserve testing
- The quality and amount of eggs accessible for ovulation are determined by this test. This series of blood and imaging tests may be given to women over 35 who are at risk of having their egg supply decreased.
- Another hormone testing
- Ovulatory hormones Thyroid and pituitary hormones which, regulate the reproductive processes.
- Imaging tests
- A pelvic ultrasound inspects the uterus and fallopian tubes for signs of uterine or fallopian tube infection or defects. A sonohysterogram, also known as a saline infusion sonogram or hysteroscopy, is sometimes used to see details inside the uterus that a standard ultrasound can’t show.
- Depending on your situation, rarely your testing might include:
- Laparoscopy
- Genetic testing
What are the treatments for female infertility?
A. Medications to restore fertility
- Fertility medicines are medications that regulate or induce ovulation. Fertility medicines are the most effective treatment for women who are unable to conceive because of ovulation complications. Fertility drugs typically work like natural hormones i.e. follicle-stimulating hormone (FSH) & luteinizing hormone (LH) that trigger ovulation.
- They are also used in women who ovulate to try to stimulate a better egg or an extra egg or eggs. Fertility drugs include:
- Clomiphene citrate
- It causes the pituitary gland to release more FSH and LH, which drive the formation of an ovarian follicle holding an egg, leading ovulation to occur. For women under the age of 39 who do not have PCOS, this is usually the first line of treatment.
- Gonadotropins
- The ovary is stimulated to generate numerous eggs by these injectable therapies. Gonadotropin medications involved human menopausal gonadotropin or hMG (Menopur) and FSH (Gonal-F, Follistim AQ, Bravelle). Human chorionic gonadotropin (Ovidrel, Pregnyl) is another gonadotropin that is utilised to develop the eggs and induce their release at the time of ovulation. With the usage of gonadotropins, there is an increased chance of conceiving multiples and having a premature delivery.
- Metformin
- Insulin resistance is a known or suspected cause of infertility in women with PCOS, and this medicine is used to treat it. Metformin aids in the reduction of insulin resistance, which can increase the chances of ovulation.
- Letrozole (Class: Aromatase inhibitors)
- It works in a similar fashion to clomiphene, causing the pituitary gland to release more FSH and LH. Letrozole is frequently given for women younger than 39 who have PCOS.
- Bromocriptine
- Bromocriptine (Cycloset, Parlodel), a dopamine agonist, may be used to treat ovulation issues caused by the pituitary gland producing too much prolactin (hyperprolactinemia).
- Risks or side effects of fertility drugs
- Pregnancy with multiples Ovarian hyperstimulation syndrome (OHSS)
- Long-term risks of ovarian tumors
B. Surgery to restore fertility
Several surgical procedures can help women conceive or increase their fertility. Surgical fertility therapies, on the other hand, are becoming less common as alternative treatments become more effective.
They are as follows:
- Laparoscopic or hysteroscopic surgery
- Correction of uterine anatomy, removal of endometrial polyps and some forms of fibroids that misshape the uterine cavity, and removal of pelvic or uterine adhesions are all options for surgery.
- Tubal surgeries
C. Reproductive assistance
- Intrauterine insemination (IUI)
- Around the moment of ovulation, millions of healthy sperm are inserted inside the uterus during IUI.
- Assisted reproductive technology (ART)
- This includes harvesting mature eggs, fertilizing them with sperm in a lab dish, and then transferring the embryos into the uterus. IVF is the most current form of assisted reproduction (ART). An IVF cycle lasts several weeks and necessitates frequent blood tests and hormone injections on a daily basis.
Read More:
For More Health Topic Click Here
Analytical Development Topic Click Here,
Formulation Development Topic Click Here,
References:
- https://www.mayoclinic.org/diseases-conditions/female-infertility/diagnosis-treatment/drc-20354313
- https://www.webmd.com/infertility-and-reproduction/guide/female-infertility https://www.ncbi.nlm.nih.gov/books/NBK556033/
- https://en.wikipedia.org/wiki/Female_infertility https://www.healthline.com/health/infertility
